CEAP Classification of Chronic Venous Disorders
Table of Contents
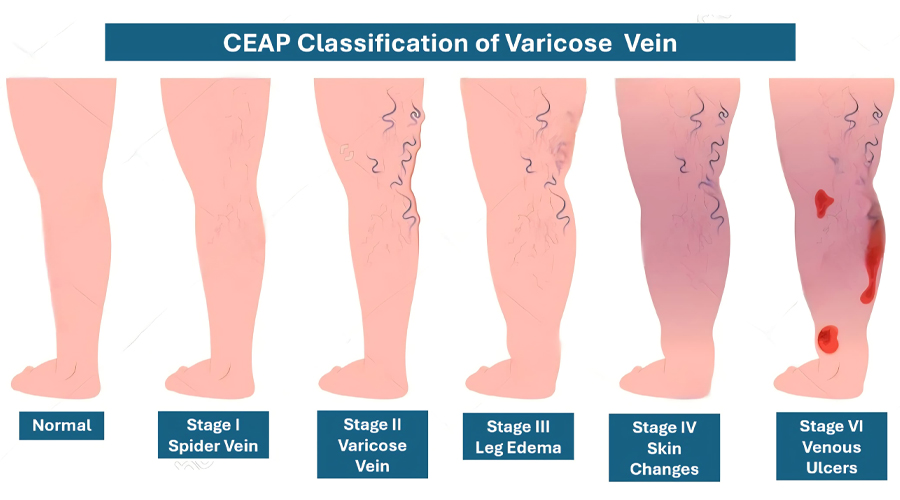
The CEAP classification is an internationally recognized system for categorizing chronic venous disorders (CVD), including varicose veins and venous ulcers. It ensures standardized diagnosis, treatment planning, and research. CEAP stands for:
- C – Clinical classification (visible signs and symptoms)
- E – Etiological classification (cause of venous disease)
- A – Anatomical classification (affected veins)
- P – Pathophysiological classification (venous dysfunction type)
Clinical Classification (C)
This classifies disease severity based on physical findings:
| Class | Findings | Symptoms |
|---|---|---|
| C0 | No visible veins | Heaviness, aching |
| C1 | Telangiectasias, reticular veins | Cosmetic concern |
| C2 | Varicose veins (≥3 mm) | Leg pain, heaviness |
| C3 | Edema | Swelling, tightness |
| C4a | Pigmentation, eczema | Brown discoloration, itching |
| C4b | Lipodermatosclerosis, atrophie blanche | Hard, woody skin |
| C4c | Corona phlebectatica | Ankle flare veins |
| C5 | Healed venous ulcer | Previous ulcer |
| C6 | Active venous ulcer | Open, non-healing wound |
Class: C0
Findings: No visible veins
Symptoms: Heaviness, aching
Class: C1
Findings: Telangiectasias, reticular veins
Symptoms: Cosmetic concern
Class: C2
Findings: Varicose veins (≥3 mm)
Symptoms: Leg pain, heaviness
Class: C3
Findings: Edema
Symptoms: Swelling, tightness
Class: C4a
Findings: Pigmentation, eczema
Symptoms: Brown discoloration, itching
Class: C4b
Findings: Lipodermatosclerosis, atrophie blanche
Symptoms: Hard, woody skin
Class: C4c
Findings: Corona phlebectatica
Symptoms: Ankle flare veins
Class: C5
Findings: Healed venous ulcer
Symptoms: Previous ulcer
Class: C6
Findings: Active venous ulcer
Symptoms: Open, non-healing wound
Etiological (E), Anatomical (A), and Pathophysiological (P) Classifications
| Code | Category | Examples |
|---|---|---|
| Ep | Primary | Idiopathic varicose veins |
| Es | Secondary | Post-thrombotic syndrome |
| Ec | Congenital | Klippel-Trenaunay Syndrome |
| As | Superficial veins | GSV, SSV |
| Ad | Deep veins | Femoral, iliac veins |
| Ap | Perforator veins | Gaiter region perforators |
| Pr | Reflux | GSV reflux |
| Po | Obstruction | May–Thurner Syndrome |
| Pro | Reflux + Obstruction | Post-thrombotic syndrome |
Code: Ep
Category: Primary
Examples: Idiopathic varicose veins
Code: Es
Category: Secondary
Examples: Post-thrombotic syndrome
Code: Ec
Category: Congenital
Examples: Klippel-Trenaunay Syndrome
Code: As
Category: Superficial veins
Examples: GSV, SSV
Code: Ad
Category: Deep veins
Examples: Femoral, iliac veins
Code: Ap
Category: Perforator veins
Examples: Gaiter region perforators
Code: Pr
Category: Reflux
Examples: GSV reflux
Code: Po
Category: Obstruction
Examples: May–Thurner Syndrome
Code: Pro
Category: Reflux + Obstruction
Examples: Post-thrombotic syndrome
How We Evaluate Varicose Veins

History Taking
A detailed history includes symptoms (pain, swelling, heaviness), exacerbating factors, past DVT, family history, and lifestyle factors like prolonged standing.
Physical Examination
- Evaluate the entire limb in supine and standing positions to assess varicosities, edema, eczema, pigmentation, lipodermatosclerosis, and ulcers.
- Palpate lower limb arterial pulses to rule out arterial disease.
Ulcer Assessment:
- Location: Typically over the medial malleolus.
- Size & Depth: Assess healing potential.
- Surrounding Skin: Look for pigmentation, lipodermatosclerosis, infection.
Doppler Ultrasound
The gold standard for detecting venous reflux, thrombosis, and perforator incompetence.

Advanced Imaging (CT/MR Venography)
Indicated for suspected deep venous insufficiency or chronic DVT.
CEAP Classification & Treatment Planning
After evaluation, patients are classified using CEAP and treated accordingly:
- C1-C2: Conservative management or saphenous ablation.
- C3-C4: Compression therapy, lifestyle modifications.
- C5-C6: Endovenous treatments (EVLA, RFA, foam sclerotherapy).
C4c – Corona Phlebectatica

A relatively newer addition to CEAP, C4c (corona phlebectatica) is a cluster of dilated venules and capillaries around the ankle, indicating advanced venous hypertension and a precursor to severe CVI.
Clinical Importance of C4c
- Predictor of Progression: Signals worsening venous disease and ulcer risk.
- Treatment Indicator: Requires Doppler evaluation and early intervention (compression, endovenous ablation).
- Differentiation: Unlike cosmetic spider veins (C1), C4c suggests underlying pathology.
